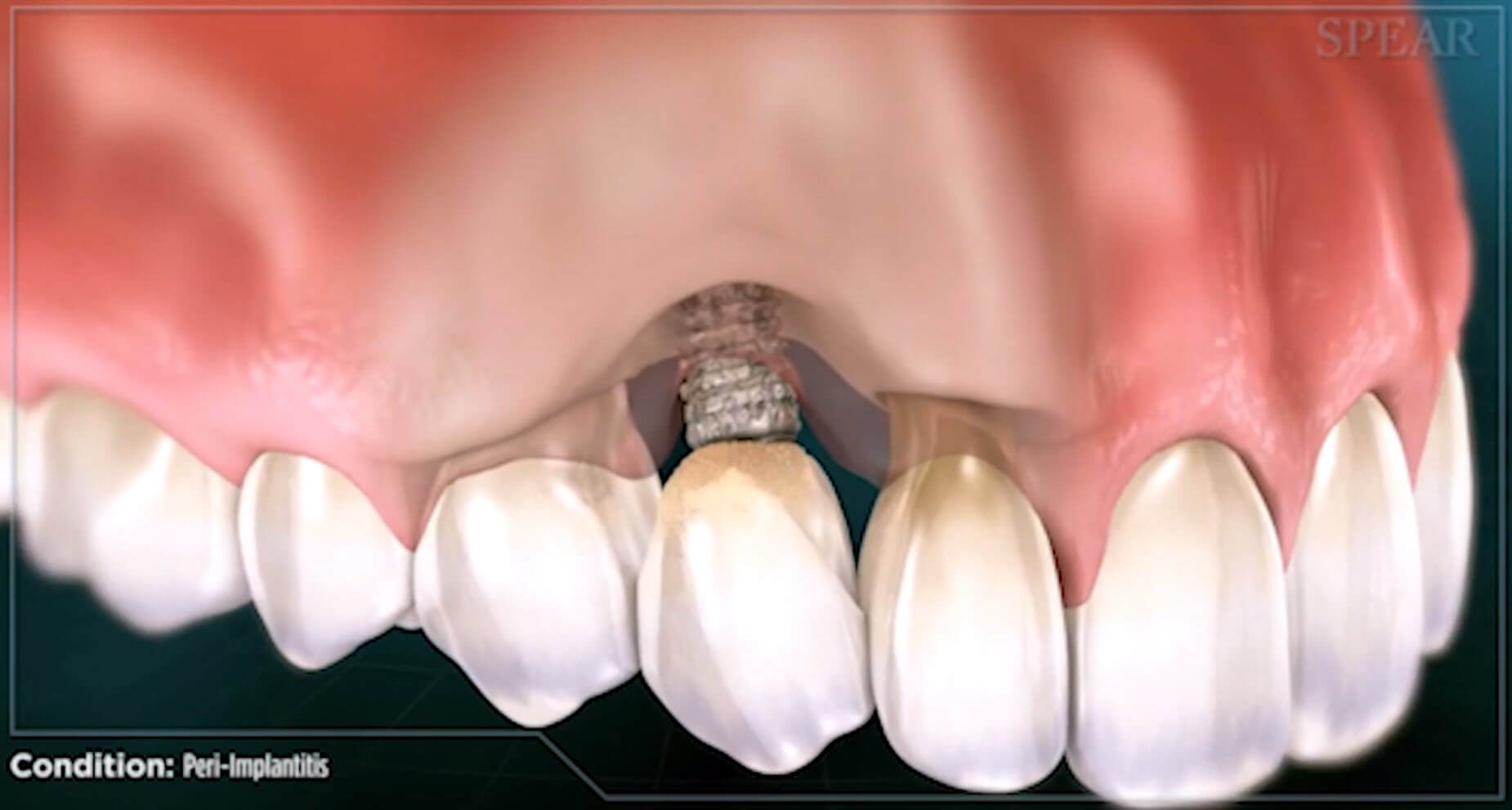
A common complication of dental implant therapy is the development of peri-implantitis (PI), which is defined as “a destructive inflammatory process affecting osseointegrated implants in function, leading to peri-implant pocket formation and loss of supporting bone”. In addition to bone loss, the clinical presentation of peri-implantitis includes deep probing depths (typically >5mm), bleeding on probing, and/or suppuration.
The reported prevalence of peri-implantitis varies greatly in the literature and ranges from 4% to 45%. However, this variability is thought to primarily reflect discrepancies in the definition of peri-implantitis across studies, rather than true differences in prevalence across populations.
A number of risk factors for PI have been identified in the literature, ranging from microbial biofilm, and design of the implant-supported prosthesis, to systemic predispositions and environmental exposures such as pre-existing periodontitis or cigarette smoking.
Clinical Research on Peri-Implantitis
In the May 2018 edition of Clinical Oral Implant Research, an article entitled, Peri-implantitis prevalence, incidence rate, and risk factors: A study of electronic health records at a U.S. dental school ; Khashayar Kordbacheh Changi used Electronic Health Records from Columbia University to study of the prevalence and risk factors for PI over a period of up to 6 years after surgical implant placement.
Results: The prevalence of PI over an average follow-up of 2 years was 34% (1/3 of all patients) on the patient level and 21% on the implant level (1/5 of all implants experience PI). Factors associated with PI in order of most significance are: ill-fitting / ill-designed prosthesis (incorrectly seated prosthesis with radiographic evidence of an open margin between implant abutment and crown, or radiographic emergence profile strongly suggestive of dental plaque retention/poor access to oral hygiene), cement-retained prosthesis and radiographic evidence of periodontitis. Also, the use of antibiotics in conjunction with implant surgery emerged as a protective exposure.
The prevalence of PI in this study is concerning, especially considering that implant therapy has been provided in an educational facility under specialty supervision. However, this study assessed longitudinal peri-implant bone level changes from the time of implant placement, while other studies employed various time points following the prosthetic restoration as a baseline reference.
Limiting the Risk of Peri-Implantitis
In general, the prevalence of PI warrants us as clinicians to do everything possible to limit this risk. My last newsletter focused on my use of 3-D surgical guides to place all implants. Having the implant placed in the most ideal position will significantly increase the likelihood of a screw-retained restoration, the best emergence profile, and a properly seated crown. All of which significantly reduce the risk of peri-implantitis.

Make sure and sign up for Dr. Kissel’s newsletter by clicking here.