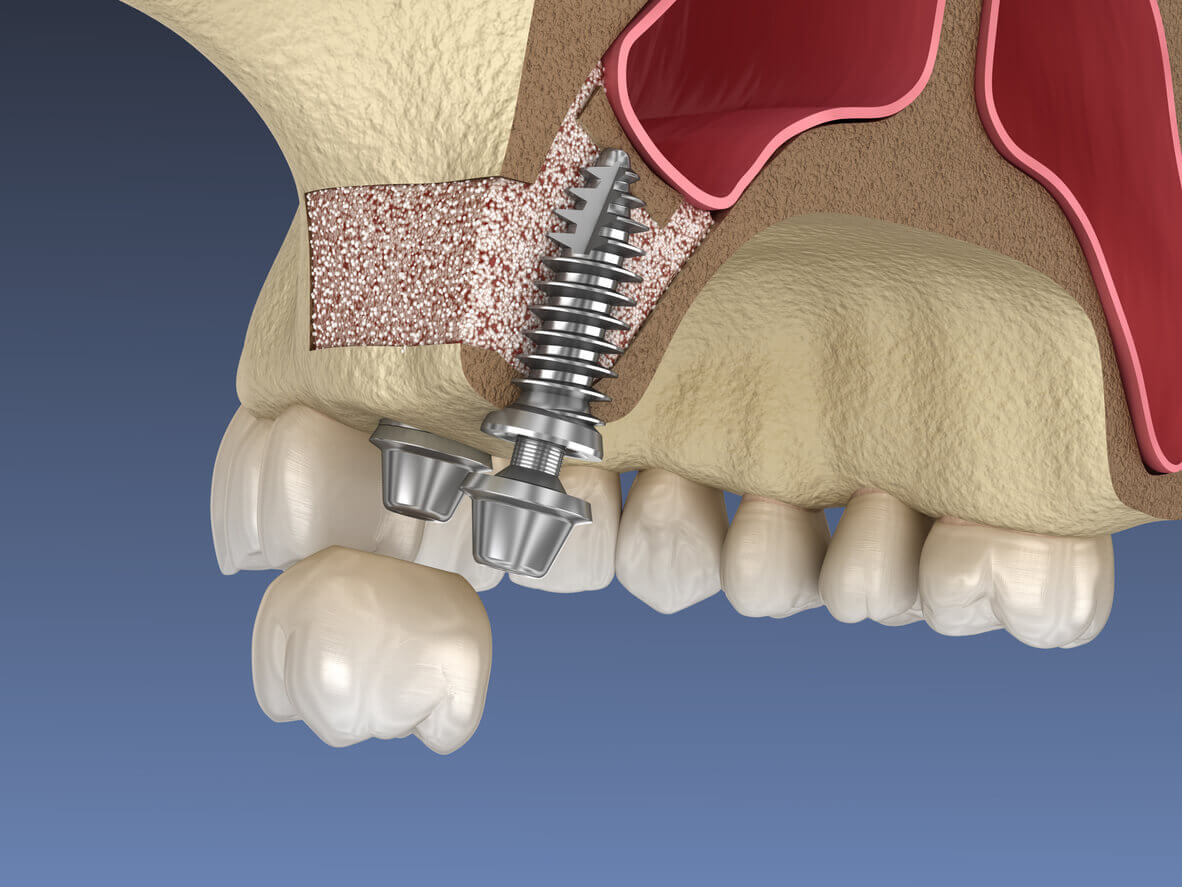
Dental implants are a common periodontics procedure, but reduced alveolar bone below the maxillary sinus is a frequent anatomical limitation to the placement of dental implants. Within the sinus cavity itself, additional anatomical structures such as septa and sinus floor slope complicate optimal implant positioning. These types of problems have been seen before at my Manhattan practice. Research indicates that the sinus lift utilizing autogenous or non-autogenous bone grafts are predictable approaches that can provide sufficient volume for implant placement.
In a general sense, a sinus lift is a surgery that adds bone to the upper jaw. Bone grafts are added, but the periodontics professional will need to move the sinus membrane up, or “lift” it. Sinus lifts may need to be used if the person has lost teeth in the upper jaw, or the anatomy of the skull might be wrong. They could suffer from advanced periodontal disease leading to bone loss, or the shape of the sinus may just be suboptimal for implant placement. In all of these cases, a periodontics professional might choose to perform a sinus lift. The bone itself can be retrieved from the patient themselves, pulled from elsewhere to be used in the sinus (autogenous), or they can be pulled from others places such as cadavers (non-autogenous).
There are two basic sinus lift techniques available to periodontics professionals: The lateral (buccal) window and the internal (osteotome) approach. In the lateral window access to the sinus is achieved through a window made in the buccal bone above the missing posterior teeth. The internal approach gains access to the sinus by drilling an implant site from the crest of bone to within 2mm of the sinus floor. Then by using a mallet and osteotome (like an awl), the sinus floor is in-fractured.
The lateral window is often utilized when there is only 1-2mm of bone remaining below the sinus, and the internal approach is used when there at least 3mm of residual bone. The lateral window is a more invasive approach often associated with significant swelling and discomfort. The internal approach is more conservative with little or no swelling and discomfort. There are two disadvantages of this approach: 1) the tapping of the mallet and osteotome on the sinus floor is not well tolerated by patients, 2) since the operator is blind to what is occurring during the creation of this in-fracture there is a higher risk of sinus membrane perforation.
Recently, using the microscope, I have modified an internal technique developed by Dr. Leon Chen and utilized it at my Manhattan practice. In essence, he drills through the sinus floor using the hydraulic pressure of air/water to cause the sinus membrane to elevate. When using the microscope, I have complete visualization of the sinus membrane through the 2-3mm wide implant site osteotomy. This significantly reduces the risk of membrane perforation and eliminates the mallet. Now sinus lifts can be performed with little to no swelling, discomfort and with greater predictability. This is a fine advancement for our patients. Below are several sinus lift cases, using both techniques.
fig. Microscopic view: Arrow pointing to sinus membrane (gray), residual bone of sinus floor noted to the right of the membrane.
Dental implants and sinus lifts are just some of the many procedures that I have been able to improve using microscopes and advanced techniques. Patients in Manhattan who visit my practice can be assured that I am at the forefront of the periodontics field, constantly looking for ways to make my practice better.
Call (212) 702-9088 or come in for a consultation, and we can discuss what we can do for you.