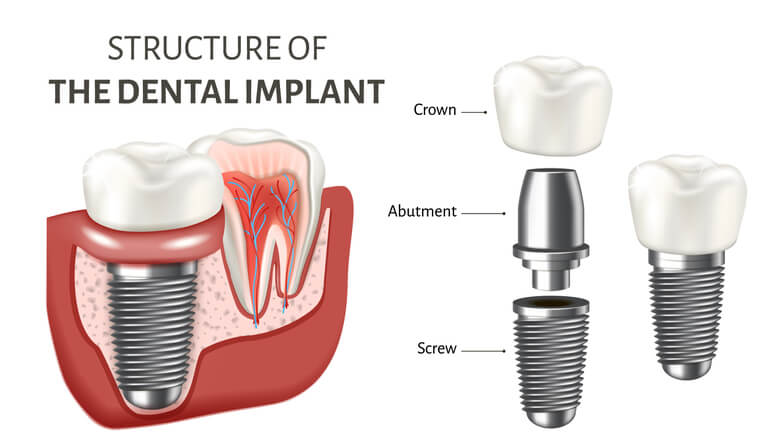
With the prevalence of peri-implantitis, dental implant abutment selection and design need to be critically assessed to minimize its impact on hard and soft tissues. Not only should a dental implant abutment be functional, but it should also be biocompatible, cleansable, and lead to an esthetic result.
In this newsletter, I would like to call attention to abutment height, gingival thickness, and dental implant position.
Dental Implant Abutment Height
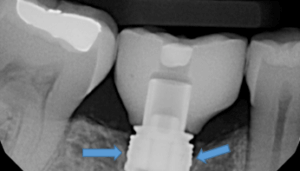
Abutment height can be defined as the distance of the crown margin to the marginal bone around the implant. This distance can significantly affect marginal bone health. An article published in Clinical Oral Implant Research, in January 2018, evaluated the interproximal marginal implant bone loss (MBL) at 3 and 6 months post-surgery. They placed definitive titanium abutments on a bone level platforms and switched dental implants at the surgery. Significant marginal bone loss was found to be greatest when short abutments, (1mm abutment height), were utilized when compared to 3mm height. Another recent randomized clinical trial in the same journal, July 2019, evaluated marginal bone loss around bone-level platform switched implants using, 3mm height abutments placed 2mm sub-crestalally and 1mm height abutments placed equicrestally. Clinical and radiological measurements were performed at 3, 6, and 12 months after surgery. Here they found that implants with longer abutments had significantly less marginal bone loss.
Results of Studies on Dental Implant Abutment
The results of these studies suggest that the shorter the prosthetic abutment height, the greater amount of marginal bone loss that can be expected with bone-level platform switched implants. When implant abutment height is less than 2mm, marginal bone loss will occur as the biologic width is re-established. Longer abutment height will allow for the reestablishment of biological width without bone loss. When the soft tissue thickness is thin, the abutment height will need to be short to achieve proper esthetics. In these cases, it is best to place the implant subcrestal (using a long abutment height for the establishment of biologic width) or build a more soft tissue height to prevent MBL.
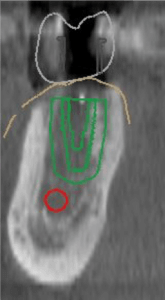
3-D Planning of Dental Implant Abutment
With 3-D planning, one can see the soft tissue height and make better choices regarding implant vertical position. If possible I would appreciate the opportunity to jointly view with you the 3-D implant workup. And discussing soft tissue height, implant position, abutment height/contour, and bone levels, prior to implant placement. If you have any questions please don’t hesitate to call.